Optimizing Your Sleep
© T.R. Morris, ND
Do you wake up feeling tired, foggy or achy? Or do you tend to have a sore throat or a headache in the morning? If so, it's likely that your sleep is disturbed or insufficient. Why is this important? Beyond just feeling tired, poor sleep is a leading cause of death and disease.
Click here to fill out your Functional Sleep Questionnaire.
Recent studies show that disturbed or insufficient sleep predictably causes overeating, weight gain, and type II diabetes. "Sleep deficiencies and circadian disruption associated with metabolic dysregulation may contribute to weight gain, obesity, and type 2 diabetes potentially by altering timing and amount of food intake, disrupting energy balance, inflammation, impairing glucose tolerance, and insulin sensitivity."(1) Other studies showed that chronic insufficient or disturbed sleep is directly linked to inflammation. (2) In this study participants were given a 4h/night sleep opportunity for for five nights and found increased levels of all the major inflammatory cytokines like hs-CRP.
According to the CDC, 35% of Americans get less than 7 hours of sleep per night.
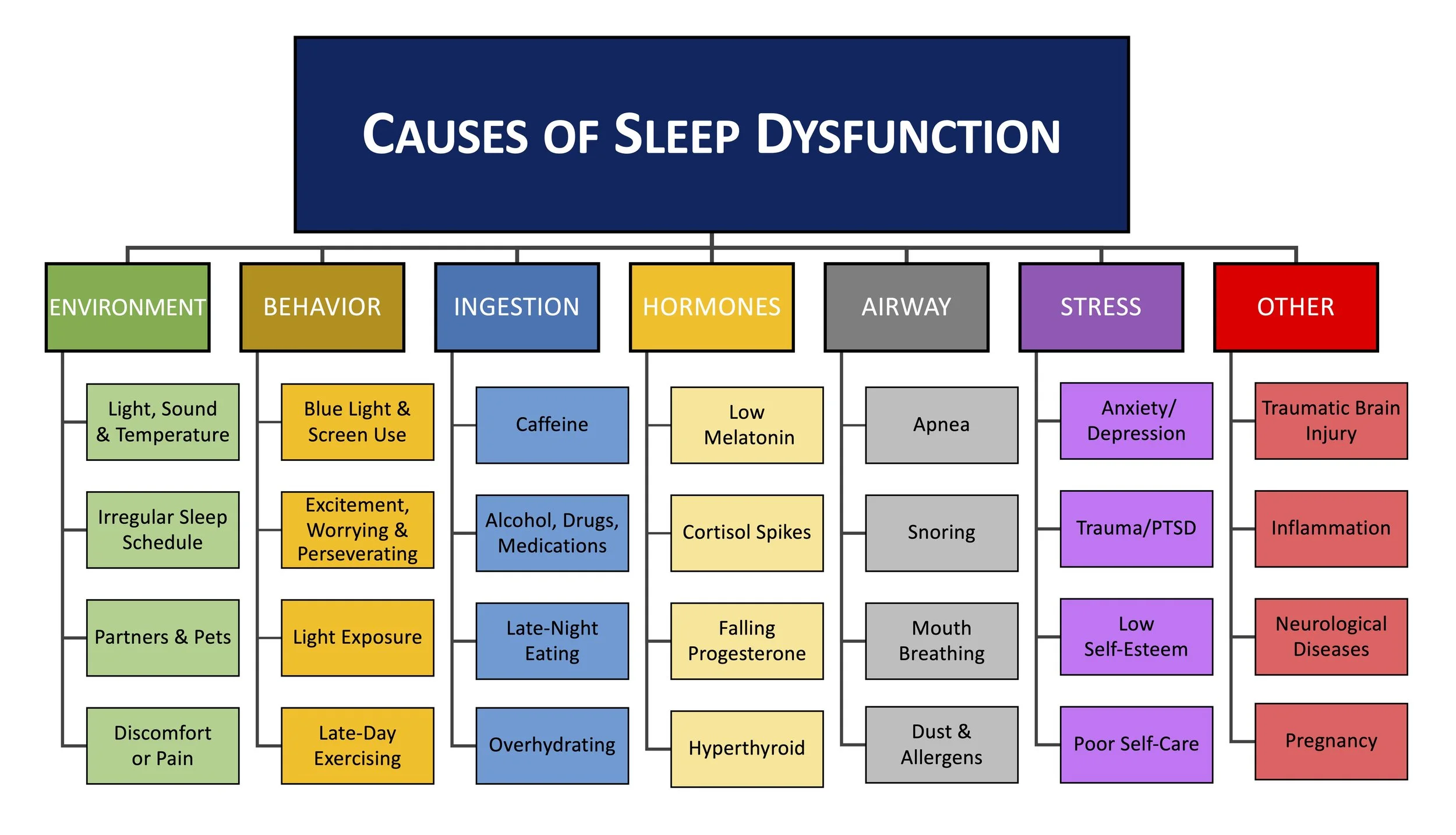
There are many things you can do to improve your sleep. These include improving your sleep environment (light, sound, bedding), limiting some activities around bedtime, moderating caffeine and alcohol intake, reducing allergens, ensuring nasal breathing, supplementing with melatonin, and many more. If you are concerned about your sleep, help is available that can give your health and vitality a major boost.
We all tend to make less melatonin as we age. This vital hormone is made in the pineal gland, and the timing is set by light exposure in the morning and the end of the day. If you are having trouble falling asleep, then quick-dissolve melatonin tablets may be for you. Taking 0.25 to 3mg 30-60 minutes before you want to be feel drowsy. Word to the wise, do not take melatonin less than 7-8 hours before you want to be awake, because this can cause morning groggyness.
If you have trouble staying asleep, then time-release melatonin tablets may help. These don't have a dramatic effect on falling asleep, but they can help prevent middle of the night wake-ups. Adults with mid night wake-ups often benefit from 1-5mg before bed.
My front-line therapy for insomnia due to an overactive mind is L-Theanine. This is a simple amino acid with a variety of health benefits. It increasing levels of the relaxing GABA and glycine levels in the brain. GABA and glycine are inhibitory neurotransmitters that work to offset overactive excitatory neurotransmitters from lingering stress or worry. Theanine promotes a state of relaxation and calm and reduces stress, anxiety, and even symptoms of ADD. Chewables or lozenges can be VERY effective. Paired with intentional breath work, L-theanine can help you find and explore a new normal of calm and relaxation at night or anytime during the day too.
There are lots of other natural options to help you sleep. L-Glycine is a natural aid to inducing faster and deeper sleep, and 0.5-3 grams before bed can make a world of difference. Magnesium-threonate is a new and highly absorbable form of magnesium that is especially relaxing to nerves and the central nervous system. It’s well worth a try.
If you are having really bad middle of the night wake-ups, especially if you are feeling alarmed or wide awake and can't fall back asleep for more than 15 minutes, it may be spikes in cortisol that are disturbing you. It could be from falling blood sugar, so having a light snack before bed can be helpful. If that does not help, you may benefit from Phosphatidylserine (PS) capsules. PS tempers evening cortisol spikes. PS dosing is tricky. Take 100-300mg at bedtime, or 100-300mg with dinner and at bedtime. Start at low doses and work your way up with this one. More is not better, and too much can paradoxically make midnight wake-ups worse. PS is not for everyone, so I save this intervention for last with really tough cases of middle of the night insomnia.
If a woman is having sleep disturbances in the second half of their cycle (after ovulation and before menstruation), falling levels of progesterone is often the cause. Supplemental progesterone can be a lifesaver. During perimenopause, a woman’s ovaries gradually (over several years) decrease production of both estrogen and progesterone.
Hot flashes at night can severely disturb sleep and may be due to falling estrogen levels. If a woman has her ovaries surgically removed (oophorectomy), menstrual cycles end abruptly and menopausal symptoms are often more severe. I often like to start with black cohosh which has a good track record of helping women from with sleep. Studies suggest it has a selective estrogenic effect, and others describe a serotonergic and dopaminergic receptor blocking effect.
When appropriate, bioidentical hormonal replacement therapy (HRT) with estrogen and/or progesterone can help immensely with sleep and other menopausal symptoms. This must be done carefully, and under the care of a skilled practitioner.
Gabapentin is a medication that is typically given for nerve pain. Low doses have an excellent effect on helping people get deeper and more restful sleep.
Another medication to consider for poor sleep quality is the tricyclic antidepressant drug, Amytrptaline. Amitriptyline inhibits reuptake of serotonin and/or norepinephrine at the presynaptic neuronal membrane, which increases concentration in the central nervous system (CNS). Amitriptyline has been shown to be effective in the treatment of REM sleep disorder behaviors.
It is Obstructive sleep apnea (OSA) is when a sleeper stops breathing for at night. OSA is usually due to the tongue and throat obstructing the sleeper’s airway. These tissues naturally relax as we slip into deeper sleep, so apnea events happen when we are least likely to notice or remember. OSA is very common and affects more than 20 million Americans. Sleep apnea can strike anyone at any age, even children, and is a serious medical condition that is directly linked to high blood pressure, type II diabetes, increasing weigh gain, heart attacks and strokes.
If you snore or wake up with a sore throat, or if your sleep became disturbed as you gained significant weight, apnea is quite likely for you. New wearable devices that record movement, sound, pulse and even O2 saturation make testing yourself at home a viable alternative to a medical sleep study.
If you think you’d know for sure if apnea was happening to you, you’re wrong. Surprisingly, most people with sleep apnea do not remember gasping for air or even sitting bolt upright in bed because these events happen right when sleepers enter the deepest levels of sleep. Apnea causes a severe disruption to your sleep as your body gets starved of oxygen and is jolted awake—dozens or even hundreds of times per night.
Risk factors for apnea include: snoring, being overweight, having difficulty breathing through your nose, swollen tonsils, a narrow throat, a large tongue. This Sleep Apnea Questionnaire can help you gauge your risk of having sleep apnea.
For simple snoring and mild to moderate sleep apnea, a simple Breathe-Right Nasal Strips can make a world of difference. Even if you don't snore or suspect apnea, many people who try nasal strips report feeling more rested and alert in the morning. They may even remembering dreams more often which indicates more efficient REM sleep. Weight loss never hurts either. In more severe cases, an oral appliance to keep your lower jaw forward or a continuous positive airway pressure (CPAP) machine may be indicated. They are not sexy, but most patients with moderate or severe apnea feel so much better on a CPAP that they never want to go without them again. Once you are sleeping better, many patients finally have the energy needed to improve nutrition and exercise habits to address the leading cause of apnea—weight gain.
Whatever the cause, if you don’t feel like your sleep is optimal, getting some professional help can drastically improve the quality of your life—and extend it.