Navigating IBS & SIBO with Functional Medicine
Click here to take Dr. Morris’s Functional Gut Health Questionnaire.
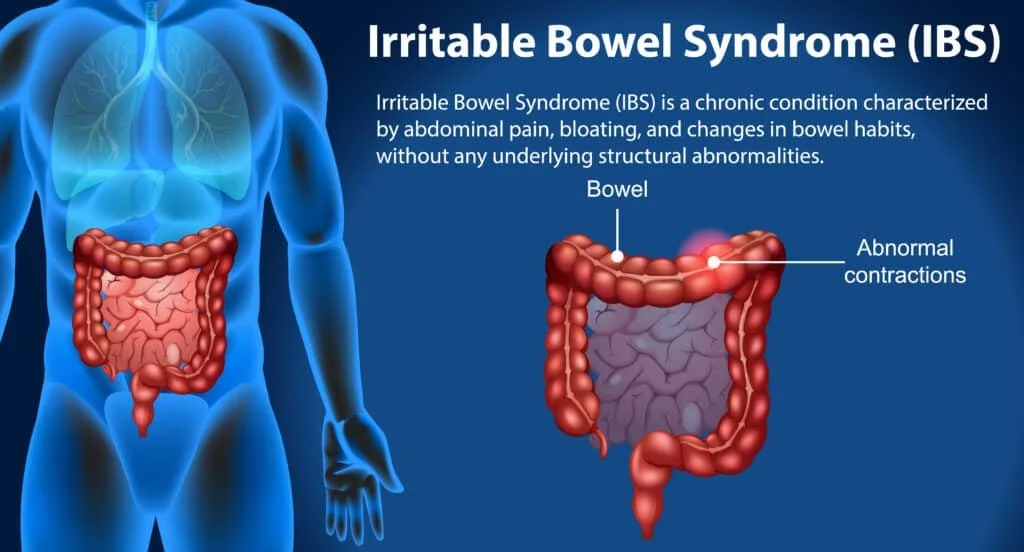
Irritable bowel syndrome (IBS): If you have abdominal pain, bloating, gas, and diarrhea or constipation then you probably have IBS. Other GI symptoms with IBS include: bowel urgency, a sense of incomplete evacuation, mucus in stool, heartburn, and a growing list of food sensitivities. Its estimated that a whopping 10-15% of American adults have IBS, and it is one of the most common disorders seen by doctors. (2) Of the 25-40 million Americans with IBS symptoms, only 1/2 to 1/3 have been diagnosed. If this is you, then help is available.
Digestive complaints in general are shockingly common. A survey of 71,000 Americans adults in 2012 found that 61% had at least one digestive complaint in the past week. That year, GI complaints in the US accounted for 105 million ambulatory care visits, 14 million hospital admissions, 236,000 deaths, and $142 billion in total costs. (1)
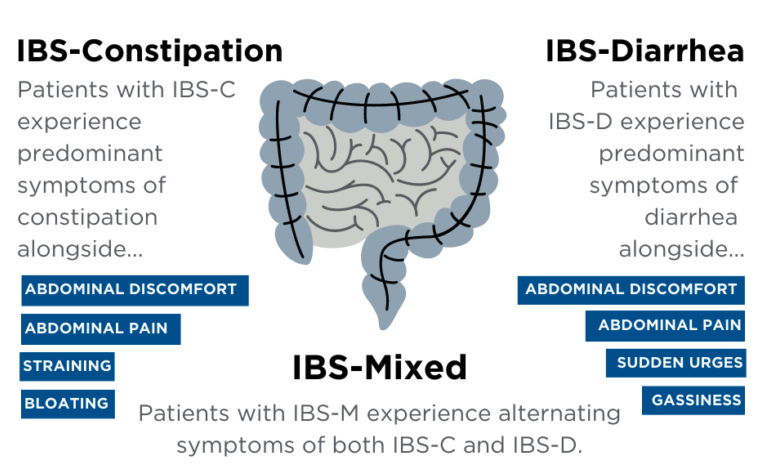
The three types of IBS
“Syndromes” like IBS are a collection of symptoms without a defined cause. Science is catching up though. We now know that “food poisoning” (bacterial gastroenteritis) is associated with an 11% chance of developing chronic post-infectious (PI) IBS. Every year, 1 in 6 adults suffer from an episode of food-borne illness in the United States, placing a great number of individuals at risk of developing PI-IBS. 8 Conservative estimates suggest that PI-IBS is 9%, which would account for over half of IBS in the United States.9
Small Intestinal Bowel Overgrowth (SIBO): 60% of IBS patients test positive for SIBO. SIBO is a diagnosable condition where elevated levels of certain gasses (hydrogen, methane, or hydrogen-sulfide) are detected in breath. The source of these gasses are problematic or overabundant bacteria in the small intestine (SI) that fermenting carbohydrates and other sugars. Anything that slows the small intestine down (infection, hypothyroid, opiates, surgical scarring, dysbiosis, low fiber diet, hormonal irregularities) can set you up for SIBO, and IBS.
Breath testing: SIBO can be diagnosed with a simple breath test. This involves involves drinking a carbohydrate solution and breathing into a tube every 15–30 minutes for 2–3 hours to collect breath samples.
What do the results mean?
Hydrogen (H2): An increase in H2 of ≥20 ppm within 90 minutes is associated with both IBS-D and methane-negative IBS-C. Higher levels of H2 correlate with abdominal pain, diarrhea, and bloating severities.” (1) H2 overproduction is most often caused by E. coli and Kelbsiella.
Methane (CH4): Intestinal methane overproduction is diagnosed when breath test methane increases ≥10 ppm at any timepoint. Intestinal methane overproduction (“IMO”) causes intense gut spasms and contributes to constipation and IBS-C. Methanobrevibacter smithii is the predominant methanogenic archaeon found in the human colon and SI. (2) .
Hydrogen sulfide (H2S): Intestinal sulfide increases of over 3.0 PPM found on breath testing at any time point is associated with IBS-D. Intestinal sulfide overproduction (“ISO”) primarily produced by Desulfovibrio (DSV) bacteria. (3) DSV are sulfate-reducing bacteria (SRB) common in the environment and within the human gastrointestinal tract. In limited quantities, SRB can be “commensal” (neither good nor bad), however, DSV can also be “opportunistic pathogens” when overabundant. H2S levels over 1.5 PPM at all time points are associated with IBS-D.
Reccomended options for SIBO testing:
H2 + CH4 Home Kit: Genova ($225)
H2 + CH4 Reusable Home Device: AIRE-2 ($249)
H2S + H2 + CH4 Home kit: Trio-Smart ($349)
What do we do with positive SIBO tests?
It should first be noted that good healthcare always starts with a complete medical history and and ruling-out other potentially more serious underlying conditions, such as celiac, and inflammatory bowel disease, hypothyroidism, GERD. That said, when you have a positive SIBO breath test, here’s what I typically recommend:
High H2: The antibiotic Rifaxamin has a good record of reducing H2 production, and reduced H2 production correlates well with reduced symptoms. With a positive H2 breath test, 56% of SIBO patients with IBS-D get better with Rifaxamin. If those patients have a negative repeat breath test after treatment, the success rate rises to a whopping 76.5%. (4) Even with no breath testing at all, 44% of IBS patients recovered.
High CH4: Neomycin + Rifaxamin therapy together x14-days reduced constipation scores significantly more than Rifaxamin alone. (5) Metronidazole works well as a substitute for neomycin. IBS-C that is methane-negative indicates a further workup for other causes of constipation.
High H2S: Bismuth has a good record of reducing H2S release in the colon. (6) Reducing the intake of high sulfur foods (brassicas, beer, wine, red meat, etc.) can also help.
While it’s nice to have a somewhat reliable treatment for IBS, a 14-day course of rifaxamin can cost $2,200-2,800 without insurance. Thankfully we have other less invasive and less expensive options to try first:
Avoiding problematic foods
Supplementing HCl & digestive enzymes
Probiotics and prebiotics
Supporting a healthy gut lining (Zinc, Glutamine, NAC, MSM, NAG, demulcents)
Natural antibacterials (berberine, garlic, oregano, thyme, peppermint)
Peppermint oil (PO) has been shown to be a safe and effective therapy for pain and global symptoms in adults with IBS. Peppermint is a carminative herb containing monoterpene compounds that relieve IBS. PO contains L-menthol, which blocks calcium channels in smooth muscle, yeilding an antispasmodic effects [9]. PO also possesses antimicrobial, anti-inflammatory, antioxidant, immunomodulating, and anesthetic activities, all of which may be relevant for the treatment of IBS. https://pmc.ncbi.nlm.nih.gov/articles/PMC6337770/
New IBS Research: The five main culprits of bacterial gastroenteritis are E. coli, Klebsiella, Salmonella, Shigella, and Campylobacter. All five of these bad bugs, produce a toxin called cytolethal distending toxin-B. CDT-B kills immune, dendritic, and epithelial cells in the gut. Worse, our antibodies to CDT-B trigger autoimmunity when they cross-react with the viniculin proteins in our intestinal nerves. Damage to these nerve interferes with GI motility and sets patients up for SIBO and IBS. Studies have shown that anti-Vinculin levels are higher in IBS-D patients, and anti-CDTB antibodies are higher in both IBS-C and IBS-D patients. (2) Lower levels of these antibodies correlate with symptom resolution. New therapies are in development.