Low-Thyroid Care: Functional Treatments
Low-Thyroid Symptom Constellation
Adequate thyroid hormone production is one of the most important factors to optimal health. In response to signals from the pituitary gland, the thyroid gland produces the T4 and T3 hormones that set the basic metabolic rate for every cell in the body. This includes brain, heart, lung, bone, muscles, your immune system, digestion, liver and kidney function and everything else.
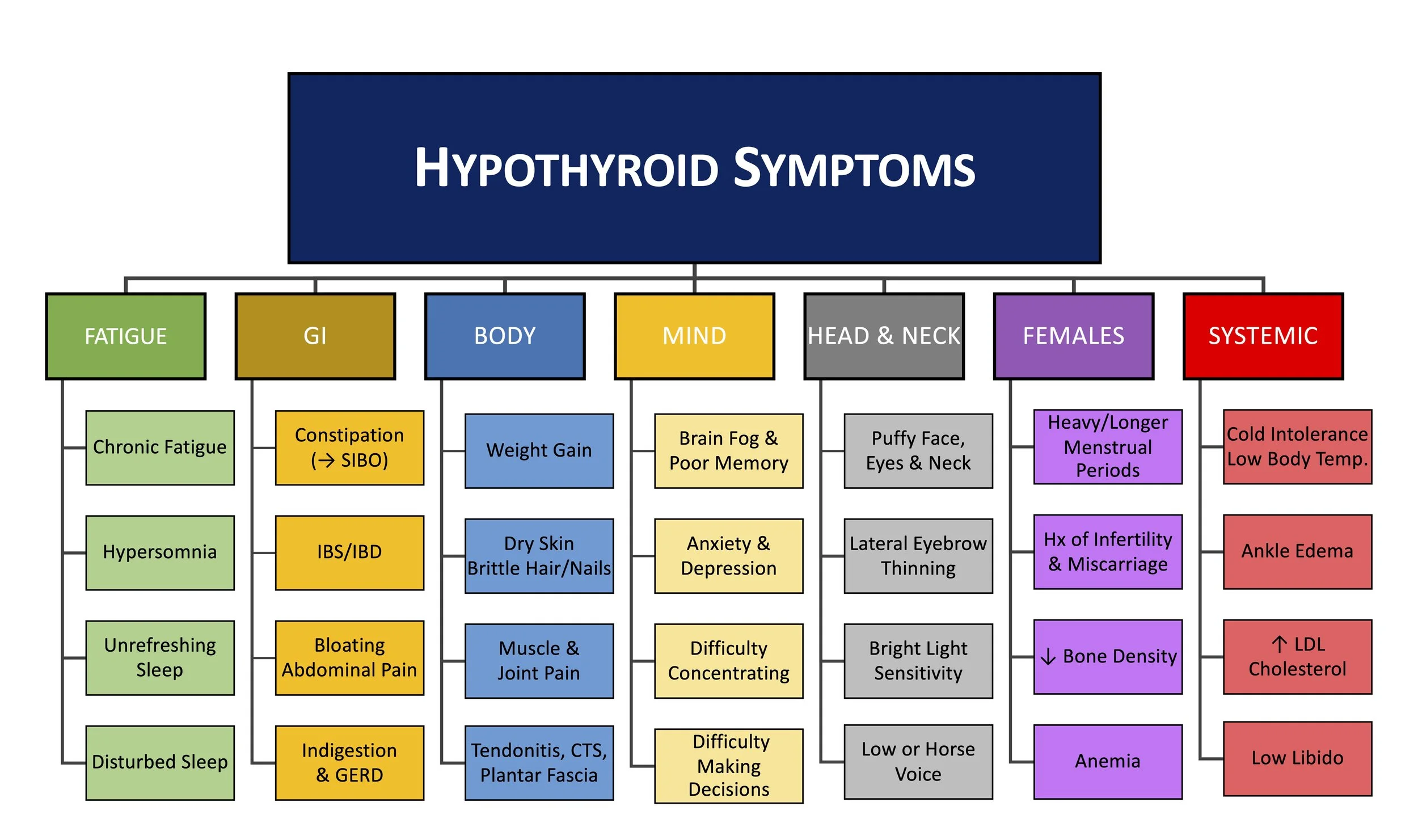
Sub-optimal thyroid function can cause a wide range of chronic or debilitating symptoms including: fatigue, depression, weight gain, brain fog, cold intolerance, hair loss, constipation, low bone density, and poor immune function.
Click here to take a free online Functional Thyroid Assessment.
With a system this important, you might think that conventional medicine would stay up to date on how to monitor this vital system. This is not the case.
Most conventional doctors will check TSH to assess thyroid function. A high TSH indicates that the pituitary gland is “yelling” at the thyroid to get to work making T4 and T3. Testing TSH not a bad start, but conventional doctors run into a HUGE problem right away with the so called “normal range” for TSH. For starters, the normal range in use by conventional doctors around the world is anything below ~4.5-5.0 mIU/L. Tragically, this number is 20 years out of date. Peer reviewed research and the major governing bodies of clinical recommendations for how to practice medicine suggest that the standard of care has missed the boat. Below are well supported recommendations that somehow, conventional labs and doctors have been ignoring for 20 years. Strike one!
2002 – American Association of Clinical Endocrinologists narrowed the serum TSH reference range to 0.3-3.0 mIU/L, lowering the upper reference end to 3.0.
2003– The National Academy of Clinical Biochemistry, Recommends a TSH upper limit of 2.5 mIU/L.
2003 – the consensus panel (Endocrine Society, American Association of Clinical Endocrinologists, and American Thyroid Association) recommended a target TSH range of 1.0 to 1.5 mIU/L in patients already receiving supplemental thyroid therapy.
The result of this drastic and institutionalized misinterpretation of TSH is that millions of people that have low thyroid symptoms (fatigue, depression, weight gain, brain fog, cold intolerance, hair loss, constipation, low bone density, and poor immune function) are told “your thyroid is totally fine” by conventional docs. The tragedy is that supporting thyroid function is easy and relatively harmless. Sadly, instead of getting the help they need, patients get told nothing is wrong with them or put on antidepressants.
Thankfully, help is available. If someone is has low thyroid symptoms and has a TSH of >2.5, then thyroid support should be considered. If someone is on thyroid support, and is still symptomatic, then it could be worth adding more thyroid support to bring their TSH between 1.5 or 1.0.
Unfortunately, there’s more trouble with the conventional approach. When someone does manage to cross the outrageously high TSH bar to get a diagnosis of hypothyroidism, the treatment they get often doesn’t work. The conventional therapy is Levothyroxine or Synthroid, which is pure T4. T4 is so weak that many call it the “storage form” of thyroid hormone. T4 must be converted into T3 to become “active”. Some people with poor T4–> T3 conversion might just need more selenium and zinc–for which deficiencies are quite common. So T4 therapy reliably lowers patient’s TSH to appear “normal”, but it may not make patients feel any better. When TSH goes down to “normal”, conventional docs often tell symptomatic patients that the problem can not in the thyroid. Strike two!
The alternative approach is to give appropriate amounts of T3 (Cytomel or Liothyronine) and T4. Another approach is to give desiccated thyroid like NatureThroid or Armour thyroid that naturally contains the ratio of both T3 and T4 that your body would naturally produce (9mcg T3 and 38mcg T4) per grain. Many patients also get benefit through decreasing inflammation through, identifying and avoiding food sensitivities, gut dysbiosis, leaky gut, and by taking curcumin and high DHA/EPA fish oil. Stress reduction and management is a huge factor that helps too.
Unfortunately, there is a third major problem with the conventional approach to cases of low thyroid function. Conventional doctors almost never consider a critical thyroid metabolite called reverse-T3 (RT3). RT3 is much like it sounds, it is a version of T3 that fits the hormonal lock, but doesn’t send the signal the body needs. It turns out that having low levels of RT3 is almost as important as having enough regular T3. The conventional range for RT3 is below 25ng/dL. If a patient is symptomatic, anything in the mid to high teens is suspicious.
Many people who are already sick (with infections, inflammation, autoimmune disease, gut dysfunction, trauma, stress, starvation etc.) can not convert T4 into T3 efficiently. So the weaker T4 sits around and gets shunted into RT3. Why does the body make RT3? In most people, RT3 is a normal byproduct of metabolizing extra T4. However, many patients chronic stress or illness (infections, inflammation, autoimmune disease, gut dysfunction, trauma, stress, starvation etc.), the body starts making extra RT3. This RT3 dominance is the body’s way of responding to high cortisol as a way to slow you down, force you to lay low, and conserve energy until the source of the stress has passed. Using RT3 as “the brakes” system evolved millions of years ago when the stressors were often temporary while many of today’s stressors don’t go away. In any event, the conventional approach of not considering RT3 is strike three!
We can assess the effect that RT3 may be having is to measure Total-T3 (TT3) and compare that to RT3. If the If a patient’s TT3:RT3 ratio is <6, some direct T3 may be indicated. Another Ratio is between the Free-T3(x100):RT3. If this ratio is <20, then this may be another indication for straight T3. So patients can have a totally normal individual thyroid lab tests, BUT if your TT3:RT3 and FT3:RT3 ratios are low then few doctors will be able to recognize that you are in fact functionally hypothyroid.
So, if you are having hypothyroid symptoms (fatigue, depression, weight gain, brain fog, cold intolerance, hair loss, constipation, low bone density, and poor immune function), get checked out and get the help you need.